Hepatitis....know it...confront it
Hepatitis is a term used for inflammation of the liver cells due to any cause
Causes of hepatitis
- Viruses: hepatitis viruses A-H, non-hepatitis viruses: herpes, cytomegalovirus etc
- Bacteria
- Parasites
- Drugs
- Chemicals & toxins including alcohol
It can manifest in two forms
Acute hepatitis
Recurrent hepatitis
Chronic hepatitis
Common routes of transmission of hepatitis are through contaminated food and drink (feco-oral route), through blood & blood products (parenteral route) and sexual contact.
Transmission through placental circulation from pregnant infected mother to child in the womb is called vertical transmission.
Acute hepatitis is characterised by abdominal discomfort, low-moderate grade fever, nausea, lethargy and loss of appetite. Most viral infections are associated with feeling of uneasiness, weakness, body pain before development of jaundice (prodrome). Jaundice is the hallmark of acute hepatitis and is usually detected by yellow discolouration of eyes and passage of dark yellow urine. Liver function tests show raised bilirubin level (mainly conjugated) accompanied by elevated liver enzymes (AST, ALT and frequently ALP). Urine shows elevated bile salts. Massive elevation of enzymes >1500 IU is rare. High fever usually indicates concurrent inflammation within the biliary system (cholangitis).
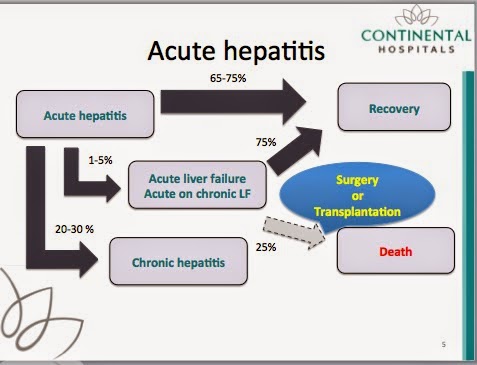
Acute hepatitis is a self-limiting disease and in most cases with supportive care, complete uneventful recovery results over a period of a few weeks. Recovery may be prolonged in elderly patients, pregnant women, those receiving medication to reduce immunity or those who have pre-existing liver damage from alcohol, fatty liver or other causes.
Alcoholic hepatitis is a unique form of hepatitis that occurs after years of large consumption of alcohol. It usually follows a binge of alcohol but can occasionally seen in early phases of abstinence.
It is a severe form of hepatitis that causes a systemic inflammatory state often associated with infection, kidney dysfunction and progression to liver failure. The underlying liver is usually pre-cirrhotic or frankly cirrhotic in patients with alcoholic hepatitis. Many patients with alcoholic hepatitis have muscle wasting and nutritional defects making them prone to infections and multi organ failure leading to significant mortality despite supportive care.
In less than 5% cases, the liver damage caused by inflammation overwhelms the body immunity and the capacity of the liver to repair and regenerate. In such situations patients may progressively and rapidly develop cardinal features of liver failure : Deep jaundice Mental changes (Encephalopathy & Clotting dysfunction. This syndrome is called Acute liver failure if patient had normal liver to start with and Acute on chronic liver failure if patient has a recognised or unrecognised chronic liver disease to start with.
Both are very severe conditions and if condition does not respond to medical measures, can be fatal.
Chronic hepatitis is usually the result of persistent or recurrent damage or the failure of immunity to clear the acute infection or insult. Chronic hepatitis is seen in 20-30% most of which is due to hepatitis B or C virus infections. Common hepatitis virus A is never chronic while less common hepatitis can rarely cause chronic infection.
Chronic hepatitis can follow an indolent course being asymptomatic for years before detection. Until liver damage has exceeded the reserve of the liver, liver function tests may be normal apart from subtle alterations.
The chronic inflammation in the liver can lead to development of primary liver cancer ( hepatocellular carcinoma) in unto 4% patients with chronic hepatitis every year.
Chronic inflammation can also lead to progressive scarring and changes in the micro architecture of the liver leading to fibrosis and eventually cirrhosis. Once cirrhosis develops, the average survival is less than 10 years in most cases. Progressive damage can lead to features of chronic liver failure like jaundice, accumulation of fluid in abdomen (ascites), clotting deficiency and mental changes (hepatic encephalopathy). Reduction in liver function reduces immunity leading to increased propensity for infections and strain on other organ systems. In such a state average survival is less than one year.
Once cirrhosis develops the risk for developing hepatocellular carcinoma doubles to 8% per year.
As in most diseases, prevention is better than cure
Prevention of hepatitis
- Consumption of safe food and drink
- Vaccination: hepatitis B, hepatitis A
- Avoid alcohol & IV drug abuse
- Avoid unprotected high-risk sexual activity
- Avoid contaminated syringes, needles, blood and blood products
- Manage body weight & keep diabetes in check
Early detection of hepatitis
- Periodic health checks
- Screening of high risk patients
- children of parents with liver cancer or hepatitis
- siblings & spouses of patients with liver cancer or hepatitis
- patients receiving blood products (haemophiliacs, thalassemics) or dialysis
- iv drug abuse history
- high risk unprotected sexual activity & commercial sex workers
- healthcare workers
- patients with suppressed immunity or those on immunity reducing drugs
Treatment of hepatitis
- Most cases of acute hepatitis need only supportive care
- No specific treatment available for most viral hepatitis except hepatitis B and C
- Inciting cause should be detected, avoided and treated accordingly
- If acute or acute on chronic liver failure results patients should receive ICU management including ventilator support: some patients who don't respond can be salvaged by urgent liver transplantation
- Measures to prevent developing chronic hepatitis & cirrhosis should be taken
- Patients with chronic hepatitis should be aggressively followed for detection of cirrhosis or development of cancer
- Early cases of liver cancer can be cured by liver surgery if there is no cirrhosis. If thesre is cirrhosis, liver transplant is the best option
- Patients with complications of liver cirrhosis can be salvaged with liver transplant
- Measures to prevent recurrence of hepatitis should be instituted even after transplant


No comments:
Post a Comment